Understanding Flesh-Eating Bacteria
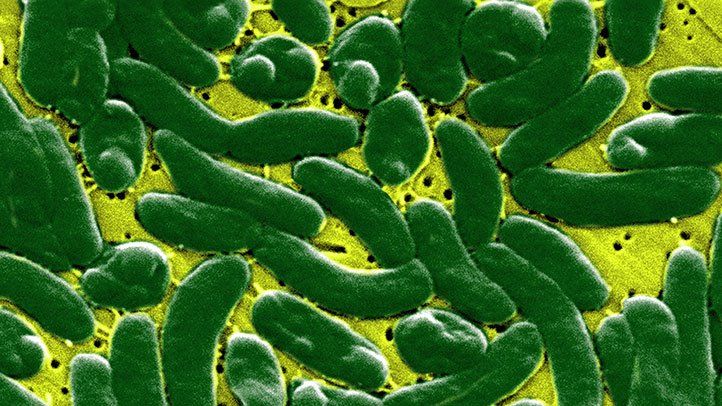
Flesh-eating bacteria, also known as necrotizing fasciitis, is a rare but serious bacterial infection that destroys muscle, skin and underlying tissue. The infection starts locally but spreads quickly, killing soft tissue as it rapidly spreads across the body. If not treated immediately, it can lead to sepsis and organ failure.
While rare, cases of flesh-eating bacterial infections seem to be increasing. Knowing the early signs and symptoms is crucial for getting prompt treatment and stopping extensive tissue damage. This article will cover the early pictures and stages of necrotizing fasciitis to help you identify and understand this rapidly progressing soft tissue infection.
What Causes Flesh-Eating Bacteria?
Several types of bacterium can lead to flesh-eating infections. The major culprits include:
- Group A Streptococcus
- Klebsiella
- Clostridium
- Escherichia coli
- Vibrio vulnificus
Many of these bacteria normally live on the skin or in the environment. An infection occurs when the bacteria enter the body through a break in the skin, such as a cut, scrape, insect bite, puncture wound, or surgical incision site. Those with a weakened immune system are most at risk.
Early Signs and Symptoms
During the early stages, a flesh-eating bacteria infection may look like cellulitis or a mild soft tissue infection. However, it progresses rapidly and can quickly become life-threatening. Early symptoms include:
- A small, red, localized infection that is warm and tender
- Severe pain and tenderness at the infection site
- Fever and chills
- Rapid expansion of the infected area
- Blisters and ulcers on the skin
- Changes to skin color, including blue, white, black or red discoloration
- Numbness at the infected site
- Fatigue and general ill feeling (malaise)
Pictures of Early-Stage Flesh-Eating Bacteria
Images of flesh-eating bacteria in the early stages show redness and swelling around the affected area. As the infection progresses, the area expands rapidly. The skin takes on a dusky red, purple, blue or black appearance as tissue dies. Here are some examples of early-stage necrotizing fasciitis:



Progression of Flesh-Eating Bacterial Infections
As necrotizing fasciitis advances, the infection spreads rapidly through fascial planes in the subcutaneous tissue. The infected area quickly expands and the borders become less defined. Here is how a flesh-eating bacteria infection typically progresses:
Stage 1: Localized Infection
Initially, the area around the infected site becomes red, swollen and painful. Flu-like symptoms, fever and chills may begin during this stage.
Stage 2: Rapid Progression
Within hours, the infected area expands and reddens. Large, fluid-filled blisters may develop as the tissue becomes necrotic. The infection spreads along the fascia. Pain becomes severe.
Stage 3: Widespread Tissue Necrosis
As it advances, the infected area continues to rapidly expand. The borders break down and infection spreads under the skin to surrounding areas. The tissue turns a blue, black or purple color as large areas become necrotic.
Stage 4: Sepsis
Without treatment, the infected tissue begins to die off and toxins enter the bloodstream, leading to sepsis and shock. Once it reaches this stage, mortality rates are high despite aggressive treatment.
Medical Imaging of Necrotizing Fasciitis Stages
In addition to a visual external exam, doctors may use medical imaging to identify and stage a necrotizing fasciitis infection. Here are some examples of what different stages look like on imaging studies:
MRI
Magnetic resonance imaging (MRI) can detect fluid accumulation and tissue edema in early necrotizing fasciitis. As the infection progresses, MRI reveals wide, thick areas of abnormal signal intensity indicating necrosis spread across fascial planes.
CT Scan
A computed tomography (CT) scan can identify fluid accumulation, gas formation and swelling of soft tissues. CT imaging can also be used to guide biopsies and surgical drainage/debridement procedures.
Ultrasound
Ultrasound allows imaging of the fascia and subcutaneous tissues. Ultrasound findings of a necrotizing soft tissue infection include thickening of the fascia, fluid collections along the deep fascia, and gas in the tissues.
X-ray
Plain film x-rays are not used for early diagnosis but may show gas in soft tissues if gangrene develops later. The rapidly progressing infection can also cause bone demineralization that is visible on x-ray.
Treating Flesh-Eating Bacterial Infections
Early treatment is critical for stopping the rapid progression of necrotizing fasciitis. Treatment involves:
- IV antibiotics - Broad-spectrum IV antibiotics are given to fight the infection.
- Surgical debridement - Surgery is done to remove infected, damaged and dead tissue.
- Supportive care - Providing IV fluids and treating shock may be needed.
In severe cases, multiple debridement surgeries may be necessary to stop disease progression. Amputation of the infected limb is sometimes required if the infection cannot be controlled.
Preventing Flesh-Eating Bacteria
While rare, necrotizing fasciitis can spread very quickly once established. To help prevent infection:
- Clean and cover any open wounds, cuts or abrasions.
- Avoid direct contact with seawater if you have an open wound.
- Thoroughly dry off after swimming and use shower shoes in public pools and locker rooms.
- Control blood sugar levels if diabetic.
- Monitor any wounds or skin infections closely for worsening.
- See a doctor for any skin infection that seems to be progressing rapidly or not improving.
Promptly seeking medical care for any signs of necrotizing fasciitis can help halt progression and improve outcomes of these aggressive soft tissue infections.
FAQs
What are the first signs of a flesh-eating bacteria infection?
Early signs include a localized red swollen area that is warm and painful. The infected area expands quickly and fever, blisters, skin discoloration, numbness, fatigue and flu-like symptoms may occur.
What does a wound with flesh-eating bacteria look like?
The infection starts as a red, swollen lesion or wound. As it progresses, the area rapidly expands, fluid-filled blisters emerge, and the tissue becomes necrotic, turning black or purple in color.
How do you detect flesh-eating bacteria early?
Carefully monitoring any skin wound or infection site for rapid expansion, worsening pain, fever, blisters and skin discoloration can help detect a developing necrotizing fasciitis infection early.
Can flesh-eating bacteria be cured if caught early?
Yes, rapid surgical debridement and intravenous antibiotics can halt the progression of the infection if administered very early in the course of the illness.
What are the stages of a flesh-eating bacteria infection?
The stages are: 1) localized infection, 2) rapid progression as infection spreads under skin, 3) widespread tissue necrosis, 4) systemic sepsis as bacteria enter the bloodstream.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a healthcare professional before starting any new treatment regimen.